If your dentist recommends root canal therapy, try not to worry — this procedure is a well-established way to relieve pain and protect your natural tooth. Advances in techniques and instruments have made contemporary root canal treatment predictable and much more comfortable than many people expect. When performed properly, it removes the source of infection or irritation and preserves the tooth so you can continue to chew, speak, and smile with confidence.
At Flossophy Dental, we prioritize patient comfort and clear communication. Our approach blends modern tools with careful attention to each individual’s needs, so you understand what’s happening at every stage of care. Root canal therapy is a restorative step designed to keep your mouth healthy while avoiding the long-term consequences that can come with extracting a damaged tooth.
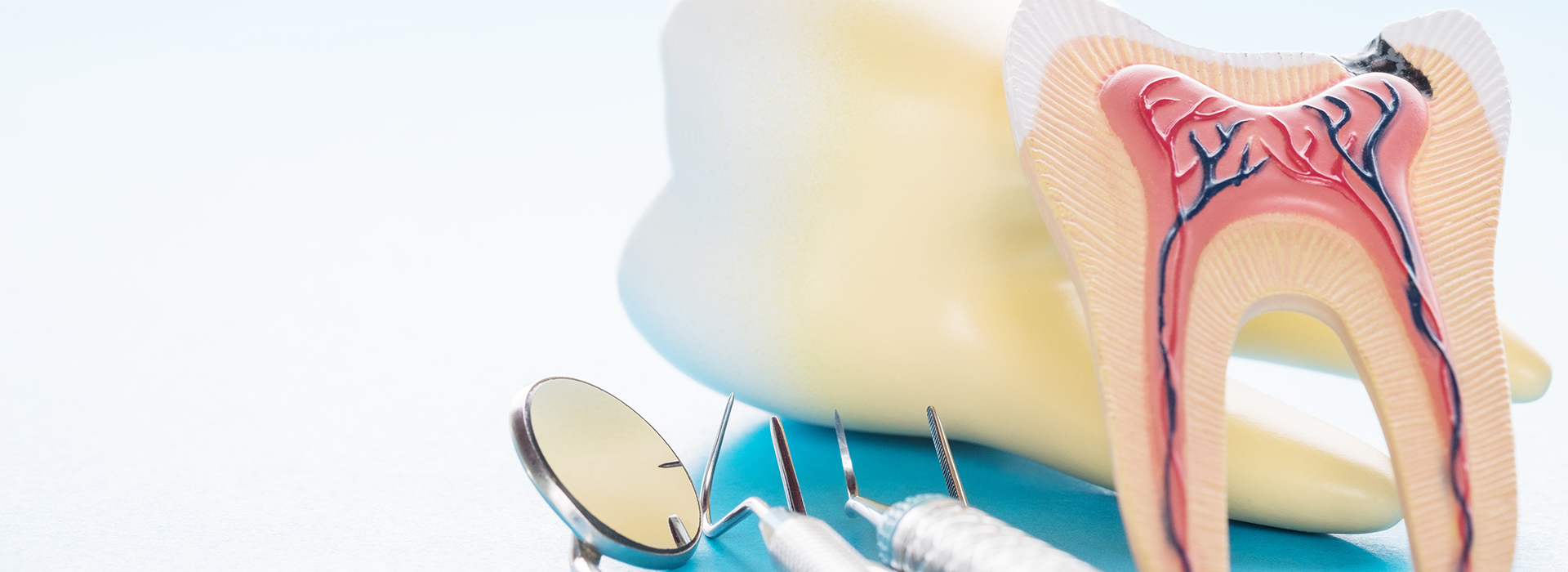
Root canal treatment has evolved significantly. With improved imaging, refined instruments, and better materials, dentists can treat the inner tissues of a tooth with high precision. The primary goal is straightforward: remove inflamed or infected tissue, clean and shape the internal anatomy, and seal the space to prevent recontamination. Preserving the natural tooth whenever possible helps maintain surrounding bone and the proper alignment of neighboring teeth.
Many patients are surprised to learn that the procedure itself is performed under local anesthesia, which blocks sensation in the treated tooth so that discomfort during the appointment is minimal. For those who experience anxiety, additional calming options can be discussed to make the visit less stressful. Most people report that the relief they feel after treatment is far greater than any temporary soreness from the procedure.
Choosing root canal therapy over extraction is often the best long-term option because it retains natural chewing function and avoids the need for replacement prosthetics. When a treated tooth is restored properly — typically with a permanent crown or similar restoration — it can serve you reliably for many years with routine care and attention.

Teeth are more than what you see on the surface. Beneath enamel and dentin is the dental pulp, a soft core of nerves and blood vessels that helps a tooth develop and sense temperature or pressure. When decay, trauma, or deep wear reaches the pulp, those tissues can become inflamed, infected, or necrotic (dead). At that stage, the tooth can no longer heal on its own and will usually require professional intervention.
Symptoms vary. Some people experience sharp, lingering pain with hot or cold, discomfort when biting, or noticeable swelling. Others may have minimal or no pain while X-rays reveal infection at the root tip. Because presentations differ, a careful clinical exam combined with appropriate radiographs helps determine whether root canal therapy is the most appropriate course.
Left untreated, an infected pulp can compromise the surrounding bone and adjacent teeth and may lead to persistent discomfort or spreading infection. The purpose of root canal therapy is to remove the problematic tissue, disinfect the internal system of canals, and seal the tooth to support long-term oral health.
Although not every toothache means a root canal is required, several indicators commonly point to the need for treatment:
If a toothache persists despite home care or reappears after short-lived relief, the underlying nerve may be compromised. Pain that wakes you at night or comes on suddenly with no obvious trigger often warrants prompt evaluation.
When foods or drinks that are hot or cold cause a prolonged, sharp reaction, it can signal that the pulp is inflamed. This sensitivity often becomes more pronounced as the problem progresses.
If chewing or even touching the tooth causes pain, the injury or infection may have reached the internal tissues. This symptom can indicate pressure within the tooth or involvement of surrounding structures.
Discoloration can be a sign that the internal tissues have deteriorated after trauma or prolonged decay. A grayish or brown tint is sometimes observed when the pulp has been affected.
A fractured tooth can expose the interior to bacteria or directly injure the pulp. Even a small crack may compromise the tooth’s vitality and necessitate treatment to prevent infection.
Swelling and pus drainage are signs of a localized infection. These findings should be evaluated quickly to control infection and protect neighboring tissues.
Advanced infection or bone loss around a tooth can reduce its support and lead to mobility. Treating the source of infection can often halt progression and allow healing of surrounding bone.

Addressing a compromised tooth sooner rather than later helps limit the spread of infection and preserves more of the natural structure. Early treatment reduces the chance of complications such as abscess formation, extensive bone loss, or the eventual need for extraction. It also often simplifies the restorative work that follows the root canal.
A routine dental exam or periodic X-rays can reveal problems before you notice symptoms. That’s why regular checkups are a valuable part of preventive care. When issues are detected early, interventions tend to be less invasive and recovery is smoother.
Postponing recommended treatment increases the risk of worsening symptoms and can make later procedures more complex. Timely root canal therapy protects your oral health and often allows you to keep your natural tooth functioning for many years.
Root canal therapy is performed with the goal of making the tooth comfortable and infection-free. After administering local anesthesia, the clinician isolates the tooth to keep it dry and visible, then creates a small opening to access the internal chambers. Specialized files are used to remove inflamed or infected tissue and to shape the canal spaces for cleaning.
Once the internal anatomy has been cleaned and disinfected, the canals are filled with a biocompatible material that seals them from future contamination. Many teeth also receive a temporary filling at the same visit; a permanent restoration—often a crown—is typically recommended afterward to restore strength and function.
The complexity of the tooth determines the number of visits required. A single-visit root canal may be appropriate for straightforward cases, while teeth with complex anatomy or active infections sometimes need two appointments to ensure the area is fully disinfected before final filling and restoration.

After treatment, many patients feel immediate relief from the acute pain that brought them in. It is normal, however, to experience some tenderness or mild soreness around the treated tooth for a few days as surrounding tissues heal. Over-the-counter pain relievers are often adequate, and your dental team will advise you on what to expect and how to manage discomfort.
Protecting the treated tooth while it is being restored is important. A tooth that has undergone root canal therapy is more brittle until it receives a permanent crown or similar restoration. Avoid hard or sticky foods on the treated side, and follow your dentist’s instructions about eating and oral hygiene during the healing period.
Follow-up visits let your dentist confirm that healing is progressing and that the definitive restoration fits well and functions properly. With proper care — routine brushing, flossing, and regular dental checkups — a root canal-treated tooth can remain a strong, dependable part of your smile for many years.
At Flossophy Dental, we focus on thoughtful, evidence-based care and clear explanations so you can make informed decisions about your treatment. If you have questions about root canal therapy, signs you’re experiencing, or the steps involved in restoring a treated tooth, please contact us for more information and to schedule an evaluation.

A root canal procedure is the best way to save a tooth that has been damaged by decay or injury and preserve your natural smile. The alternative is an extraction and treatment to replace the tooth. While at times a tooth is non-restorable and an extraction is the only option, when possible, it’s best to try and save your natural tooth. With proper care, a tooth with root canal therapy can serve your smile well for many years to come.
Despite lingering myths from before the age of modern dental anesthesia and technology, having a root canal procedure today is as routine and comfortable as visiting the dentist for a filling. While the procedure is performed under local anesthesia with your tooth completely numbed, we can also discuss options in dental sedation.
Whether the symptoms of a dental infection subside after a course of antibiotics, a draining abscess provides you with some temporary pain relief, or a tooth with radiographic evidence of pathology has not yet developed symptoms, it’s essential, before an infection worsens or occurs, to have a root canal procedure performed. In this way, the tooth can be disinfected, filled, and sealed to protect your health and avoid further problems.
If you have sustained a dental injury, have a toothache, jaw pain, swelling, or are experiencing any other unusual and uncomfortable oral symptoms, contact our office immediately for care. Dental problems that have not been evaluated and treated can significantly worsen, producing more severe damage and consequences for the involved teeth, your oral health, and even your overall wellbeing. Once you get in touch with our office, our friendly and compassionate office team will get you in for care at your earliest convenience.
While some root canal procedures can be completed in one visit, others may involve 2 or 3 appointments. How long it takes depends on various factors, including active infection, the number of canals in the tooth, and the tooth’s location or anatomy.
With a success rate that exceeds 95%, root canal therapy remains the most effective procedure to save a tooth in which the inner vital tissues have been damaged. However, as with all healthcare procedures, there are a small percentage of cases where the teeth become symptomatic a second time. The good news is that many of these teeth can still be saved with root canal retreatment or a minor surgical procedure known as an apicoectomy.
The best ways to maintain a tooth with root canal therapy are to get the proper restoration required to rebuild and protect the tooth, maintain proper oral hygiene, and schedule appointments for routine dental checkups and care.
Saving a tooth with root canal therapy is a wise investment that, in the long run, is typically less costly and invasive than having the tooth extracted and replaced with a fixed bridge or implant. As far as the exact cost of care, it can vary depending on which tooth is being treated. Many dental insurance plans provide coverage for root canal therapy. At the office of Flossophy Dental, we do our best to optimize your dental benefits and minimize your out-of-pocket expenses. Our staff will answer all your questions about the cost of care and discuss all your payment options.
At the office of Flossophy Dental, we use the latest technology and most effective methods of care to provide precise and gentle care. Our reputation for excellence is based upon a consistent record of achieving successful treatment outcomes while providing prompt, stress-free, and convenient treatment for every type of dental need.
Root canal therapy is a clinical procedure that removes inflamed or infected pulp from the interior of a tooth to relieve pain and stop the spread of infection. The clinician cleans and shapes the root canal system, disinfects the space, and seals it with a biocompatible material to prevent recontamination. The primary goal is to preserve the natural tooth so you can continue to chew, speak and smile with stability.
Modern techniques and imaging have made the procedure more predictable and comfortable than in the past, and treatment plans are customized to each tooth's anatomy. Local anesthesia is used to block sensation during the appointment, and calming options can be discussed for patients with anxiety. After therapy, a permanent restoration such as a crown is often recommended to restore strength and function.
Symptoms that commonly indicate the need for evaluation include persistent or severe toothache, heightened sensitivity to hot or cold that lingers, pain when biting or pressure is applied, and noticeable swelling or drainage near the tooth. Some teeth, however, show minimal or no pain while X-rays reveal infection at the root tip, so clinical examination and radiographs are important diagnostic tools. Discoloration, visible cracks or a history of trauma can also signal internal damage to the pulp.
If you experience any of these signs, prompt assessment by a dental professional can determine whether root canal therapy or another treatment is appropriate. Early diagnosis often reduces the complexity of care and limits the risk of complications such as abscess formation or bone loss. Your dentist will explain findings, review options and recommend a treatment pathway based on the tooth's condition and your overall oral health.
At the start of the appointment the tooth is numbed with local anesthesia and isolated to keep the area dry and visible. The clinician creates a small access opening, uses specialized instruments to remove infected or necrotic pulp, and shapes the canal spaces to allow thorough cleaning and disinfection. Once cleaned, the canals are filled with a stable, biocompatible material and a temporary or permanent seal to prevent reinfection.
Some straightforward cases can be completed in a single visit, while teeth with complex anatomy or active infection may require two appointments to ensure adequate disinfection. A follow-up restoration, commonly a crown, is often recommended to restore structural integrity and protect the treated tooth. Your dental team will review what to expect during the visit and any instructions for post-treatment care.
Root canal treatment itself is performed under local anesthesia, which significantly reduces or eliminates pain during the procedure. Many patients compare the sensation to having a routine filling once the tooth is properly anesthetized, and clinicians offer additional calming options for anxious patients. Discomfort after the appointment is typically mild and temporary, managed with over-the-counter analgesics and proper home care.
Occasional soreness or tenderness around the treated tooth can last a few days as surrounding tissues heal, but persistent or worsening pain should be reported to your dentist promptly. Effective communication about your symptoms helps the team address inflammation or other issues quickly. The relief from eliminating the source of infection is often substantial compared with the pre-treatment pain that brought patients in.
Preserving a natural tooth maintains chewing function, helps protect surrounding bone, and preserves the alignment of neighboring teeth. Extraction can create additional restorative needs such as bridges, implants or partial dentures to replace the missing tooth, which may increase the complexity of future care. When a treated tooth is restored properly, it can continue to function reliably for many years with routine maintenance.
Choosing root canal therapy over extraction is typically a conservation-minded approach that aims to retain natural structure and avoid the long-term consequences of tooth loss. Your dentist will weigh the tooth's prognosis, structural integrity and overall oral health when recommending the best option. If a tooth is not a good candidate for preservation, the team will explain why and discuss appropriate alternatives.
Many teeth benefit from a protective restoration such as a crown after root canal treatment because an endodontically treated tooth can be more brittle and prone to fracture. A crown restores form and function, helps distribute biting forces evenly and seals the tooth against bacterial contamination. The recommendation depends on factors such as the amount of remaining tooth structure, the tooth's location in the mouth and the planned long-term use.
In some cases a permanent filling or onlay may be sufficient, particularly for small posterior or anterior teeth with minimal structural loss. Your dentist will discuss the restorative options and timing, ensuring the chosen restoration provides durable protection for the treated tooth. Follow-up visits confirm that the definitive restoration fits correctly and that healing is progressing as expected.
While root canal therapy has a high success rate, failure can occur if bacteria remain in complex canals, if a new decay allows contamination, or if a restoration fails to properly seal the tooth. Signs of persistent or recurrent infection include ongoing or worsening pain, swelling, a sinus tract or drainage, and radiographic evidence of a persistent lesion at the root tip. In some cases, symptoms may be subtle while X-rays reveal unresolved pathology.
If a treated tooth shows signs of failure, retreatment, surgical endodontics (apicoectomy), or extraction may be considered based on the underlying cause and prognosis. Timely assessment helps determine whether conservative retreatment can resolve the issue or whether alternative care is needed. Regular recall appointments allow monitoring of healing and early detection of problems.
Alternatives depend on the tooth's condition and may include extraction followed by replacement with an implant, bridge or removable prosthesis, or in select cases, monitoring if the pulp issue is reversible. Extraction removes the source of infection but introduces the need for replacement to restore function and esthetics. The best option balances the tooth's long-term prognosis, your overall oral health and personal preferences.
Your dentist will explain the risks and benefits of each approach and help you make an informed decision that aligns with your goals. When preservation is feasible and clinically appropriate, root canal therapy is often recommended to retain the natural tooth. If removal is necessary, the team will outline restorative pathways to reestablish comfort and function.
In the days following treatment, maintain gentle oral hygiene, avoid chewing on hard or sticky foods on the treated side and follow any specific instructions from your dentist. Over-the-counter pain relievers can manage expected soreness, and you should contact the office if you experience severe or increasing pain, prolonged swelling or other concerning symptoms. Keeping the temporary material intact until the definitive restoration is placed helps protect the canal seals.
Once the permanent restoration is placed, ongoing care is the same as for any natural tooth: regular brushing, flossing and routine dental checkups and X-rays to monitor long-term success. A well-restored, endodontically treated tooth can remain functional for many years with appropriate maintenance. Your dental team will schedule follow-ups to ensure healing and restoration performance.
Preventive measures such as daily brushing with fluoride toothpaste, flossing, using an antimicrobial mouthrinse when recommended and attending regular dental exams help reduce the risk of decay and gum disease that can lead to pulp involvement. Early treatment of cavities, prompt attention to dental trauma and wearing protective mouthguards for contact sports also lower the chance of internal tooth damage. Good oral hygiene combined with professional care allows problems to be caught before they progress to the pulp.
Your dental team will advise personalized prevention strategies based on your oral health, diet and risk factors, and they can provide guidance on sealants, fluoride treatments or restorative care when appropriate. At Flossophy, we emphasize preventive care and clear communication so patients understand how to protect their smiles and minimize the need for invasive treatment. Regular visits allow the practice to detect issues early and recommend conservative measures to maintain long-term dental health.

Ready to schedule your next dental appointment or have questions about our services?
Contacting Flossophy Dental is easy! Our friendly staff is available to assist you with scheduling appointments, answering inquiries about treatment options, and addressing any concerns you may have. Whether you prefer to give us a call, send us an email, or fill out our convenient online contact form, we're here to help. Don't wait to take the first step towards achieving the smile of your dreams – reach out to us today and discover the difference personalized dental care can make.